How Dartmouth Health Uses Process Modeling to Predict the Unpredictable
Dartmouth Health is a leading academic health system in New Hampshire with a strong commitment to continuous improvement and patient-centered care. At the height of the COVID-19 pandemic, their teams were forced to pivot rapidly—transforming traditional care delivery models while ensuring high-quality outcomes and operational resilience. That’s when their Operational Excellence (OPEX) team discovered a powerful tool to support their mission: MoreSteam’s Process Playground.
From “We Think” to “We Know”
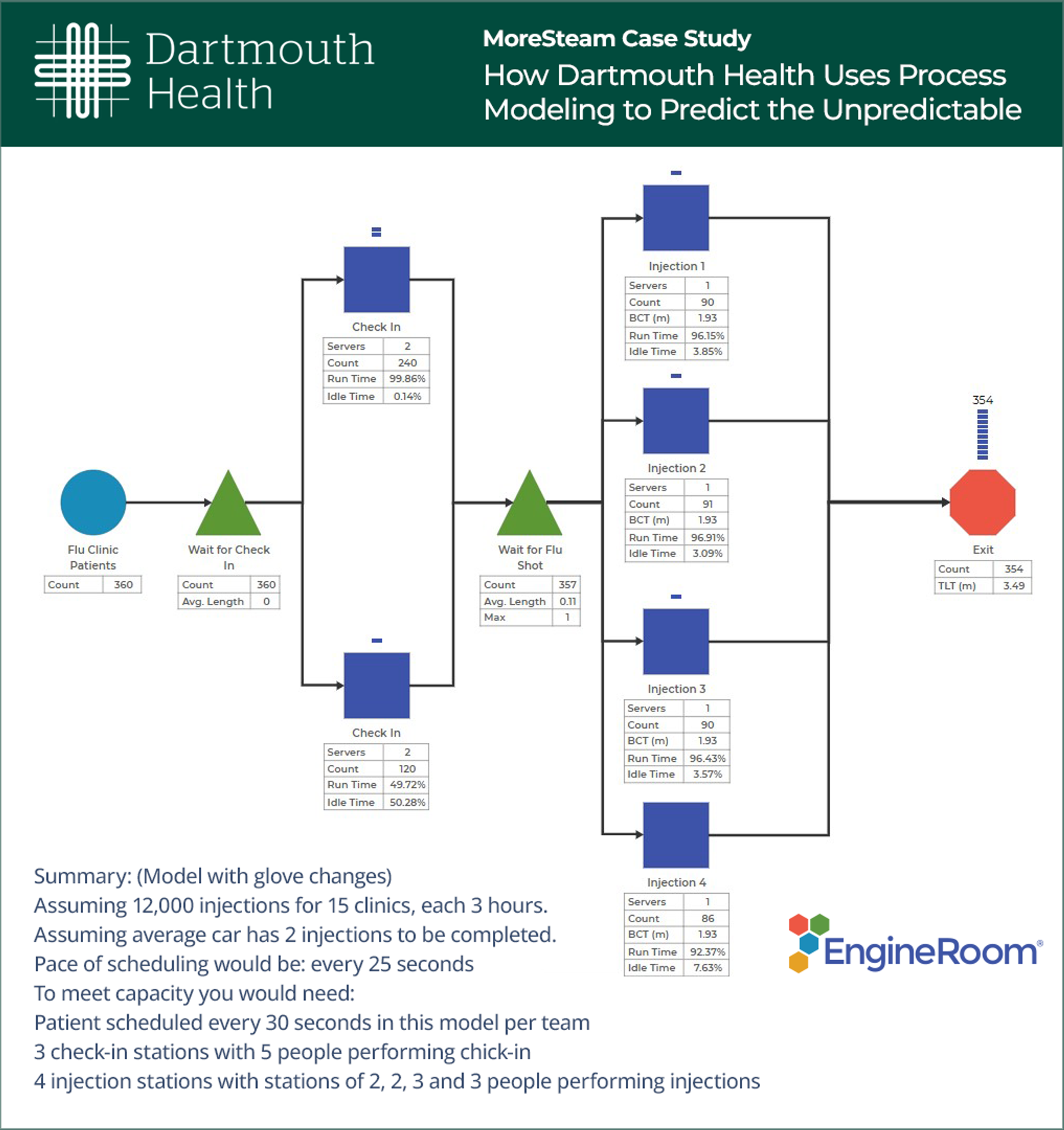
The OpEx team’s first experience with Process Playground came at a critical moment—when Dartmouth Health was redesigning flu clinics to operate as drive-throughs. They needed to quickly determine how to safely and efficiently serve patients in cars instead of exam rooms, without trial-and-error delays.
Jamie, a member of the OpEx team, and his colleague Matt used Process Playground to build a model of the proposed drive-through clinic—mapping out steps, collecting time data, and running simulations. What they discovered was a revelation. Jamie explains,
We threw the process into the simulation and immediately said, ‘This won’t work.’ We were able to show that our check-in process would create a 155-car queue unless we doubled staffing.
Instead of running a flawed pilot, they used the simulation to make evidence-based changes upfront—saving precious time when time was of the essence.
A Tool for Complex, Human-Centered Work
Since that first project, Dartmouth’s OpEx team has applied Process Playground across a wide range of operational and clinical problems:
- Flu + COVID vaccine injection scenarios (modeling staffing based on patient mix for each vaccine)
- MRI trailer rental decisions (evaluating whether to add equipment or expand staffing)
- Lab scheduling (tuning resources to balance turnaround time and technician workload)
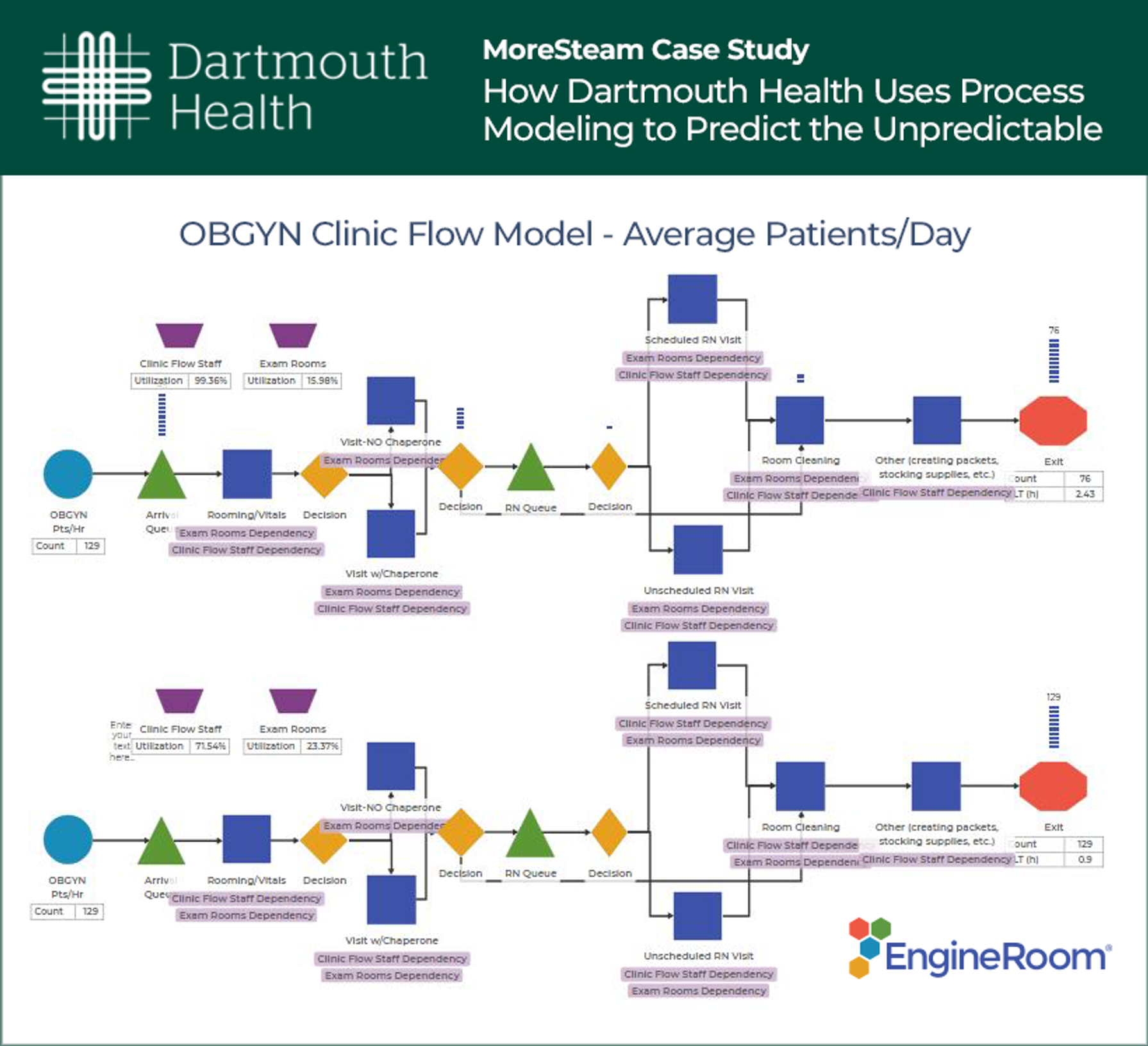
- OB/GYN staffing (defining how many staff are needed to meet 95% chaperone coverage)
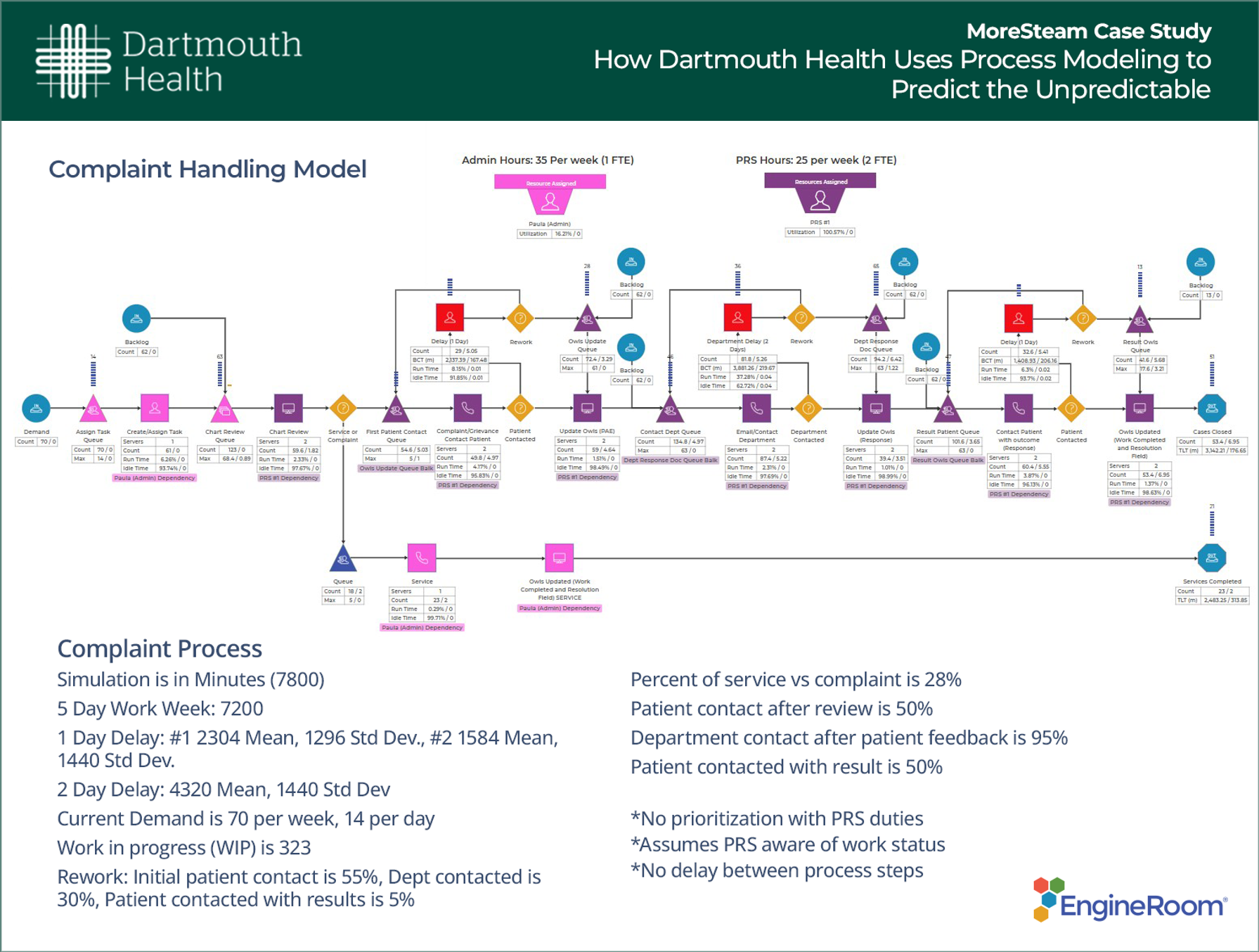
- Complaint resolution process (pinpointing delay drivers to improve patient feedback cycles)
Each model enabled the team to run scenario tests and determine the efficacy of proposed solutions without impacting day-to-day operations. Jamie adds,
It’s especially helpful in healthcare because we have so much variation. Whether it’s staffing, patient needs, or arrival times—this tool helps us understand the reality, not just the average.
Empowering Change in a Resource-Constrained System
At Dartmouth Health, the OpEx team is small but mighty: a centralized group of just a few people, pulled into high-priority initiatives across the organization. They begin projects not to “build a simulation,” but to help teams solve tough and problems. In some cases, Process Playground becomes the key to discovering the path forward. Another team member, Raquel, shares,
People reach out with a problem. We help them define the process, collect data, and then use modeling to test what’s possible.
From senior leadership to front-line staff, the models have helped people "see" why certain goals can’t be met—unless hidden delays, bottlenecks, or staffing gaps are addressed.
Teaching the Skill, Not Just Delivering the Solution
Recognizing the potential to scale this capability, the OPEX team has begun creating internal training to teach others how to prepare for modeling engagements—including process mapping, defining variation, and collecting relevant timing and capacity data. Jamie notes,
The actual model build doesn’t take long—it’s the prep work that matters. If more teams can come to us with that foundation, we can partner more efficiently and expand the reach of modeling.
Raquel, who is actively learning the tool, added, “There’s a learning curve, but with mentoring, it clicks. It’s so powerful. I wish I had this tool back when I was a practice manager.”
Why It Works: Patient Focus and People Preservation
What sets Dartmouth’s use of Process Playground apart is the intent behind every project: improving care and preserving the people who deliver it.
Every simulation is built not just to optimize flow or reduce costs—but to ensure patients are served well and staff are not burned out by unsustainable workloads. Jamie explains,
Burnout is real. We use this tool to show teams and leaders where the stress lives in a process, so we can change it before it harms the people doing the work.
Looking Ahead
Dartmouth Health’s OPEX team is continuing to build modeling capability, train more users, and integrate simulation thinking into everyday problem-solving. Their journey proves that process modeling doesn’t need to be reserved for expert data scientists—when paired with the right training and mindset, it can empower healthcare professionals to make smarter, faster, more compassionate decisions.
It’s not about throwing more resources at a problem. It’s about understanding your system so deeply that you know what really needs to change.
James Perry, LSSBB, is a Senior Performance Improvement Consultant at Dartmouth Health, where he leads improvement projects, coaches Green Belts, and teaches through the Value Institute. With a background in occupational therapy and certifications in Lean Six Sigma and hand therapy, James brings over two decades of healthcare experience to his work in Operational Excellence. James completed his Lean Six Sigma Black Belt training through MoreSteam's Blended Black Belt Certification Program.
Raquel A. Chase-Kelly, LSSBB, is a Performance Improvement Consultant at Dartmouth Health, leading improvement projects, coaching Green Belt candidates, and teaching through the Value Institute. With over seven years in ambulatory operations administration, she has managed surgical sections including Vascular Surgery and Cardiac Surgery. Raquel completed her Lean Six Sigma Black Belt training at Dartmouth College's Thayer School of Engineering.

MoreSteam's Enterprise Process Improvement platform includes the tools, training, and software you need to transform your organization, large or small, into a problem-solving powerhouse. Our products are trusted by over half of the Fortune 500 and by other organizations and universities worldwide. When you partner with MoreSteam you gain a team dedicated to helping you succeed.

Dartmouth Health's mission is to advance health through research, education, clinical practice, and community partnerships, providing each person the best care, in the right place, at the right time, every time.
Key Facilities and Services
- DHMC: 460-bed academic hospital; New Hampshire’s only Level I Trauma Center and air ambulance.
- Cancer Center: NCI-designated, advanced care and research.
- Children’s: NH’s only full-service children’s hospital.
Notable Impacts
✔ Prevented operational failures before pilots
✔ Informed staffing decisions with data
✔ Helped secure HR resources for patient care
✔ Highlighted hidden delays and burnout risk
✔ Empowered frontline teams with simulation insight
Team Philosophy
“People-first problem solving” – every model is built to improve patient care and protect staff well-being